About Cushing’s
What do you need to know about Cushing’s Syndrome?




What do you need to know about Cushing’s Syndrome?
Cushing’s syndrome is an uncommon condition caused by high levels of cortisol. There are only 0.7–2.4 new cases per million around the world every year, and it is estimated that only 40 in 1,000,000 people suffers from Cushing’s syndrome.1 Cushing’s syndrome is more common in women than in men and most often affects adults between 30 and 50 years old.11
Cushing’s syndrome describes a cluster of specified conditions, some of which involve the adrenocorticotropic hormone (ACTH) and some that do not. ACTH is a hormone that is made by the pituitary gland, a pea-sized gland located at the base of the brain.2
The most common cause of Cushing’s syndrome is a tumor that produces too much of the hormone ACTH, which in turn causes the adrenal glands to produce too much cortisol. This takes two distinct forms:2
- Cushing’s disease: caused by a benign tumour in the pituitary gland
- Ectopic syndrome: caused by a tumour found outside the pituitary gland
There are also forms of Cushing’s syndrome that do not involve the hormone ACTH and are instead caused by too much cortisol being produced directly by the adrenal glands, but these are less common.2
This page lays out key information about Cushing’s syndrome, including what Cushing’s Syndrome is and what causes it, and the impact its symptoms can have on patients’ lives. It aims to provide a foundational understanding of Cushing’s syndrome for patients and carers.
What causes Cushing’s Syndrome?
One of the reasons Cushing’s syndrome is so burdensome is because its signs and symptoms can affect nearly every part of the body. This is because Cushing’s syndrome occurs when your body makes too much of a hormone called cortisol.2 Under normal conditions, cortisol plays a variety of roles in your body including regulating various important functions in the body.
It regulates our stress responses, blood sugar and blood pressure, and inflammation, and helps our body use key nutrients. When there is too much cortisol, the body can’t work like it usually does, and essential bodily processes are thrown out of balance. Since excess cortisol can affect everyone differently, the signs and symptoms of Cushing’s syndrome can be very different person-to-person. They can affect both the mental and physical health of patients.3
The longer someone is exposed to high cortisol levels, the greater their risk of developing severe conditions as a result of Cushing’s syndrome. These conditions are known as comorbidities, and often include high blood pressure (hypertension), diabetes, fatigue and depression, all of which contribute to the burden of Cushing’s Syndrome.4
Building a life that accommodates Cushing’s Syndrome can be challenging, and often means needing extra support to help manage the daily impact of the disease.
Building a life that accommodates Cushing’s Syndrome can be challenging, and often means needing extra support to help manage the daily impact of the disease.
Understanding the signs and symptoms of Cushing’s Syndrome
Cushing’s syndrome causes symptoms that can appear different from one person to another and affect every part of daily life, including relationships, self-image, and mental and physical wellbeing.
The main symptoms that are strongly associated with Cushing’s syndrome include:2,4
- Red face
- Easy bruising
- Stretch marks
- Proximal muscle weakness
- Rounding of the face
- Excessive body and facial hair
- Acne
- Weight gain
- Fat pads on back, neck and collarbone
Diagnosis is not always a simple process
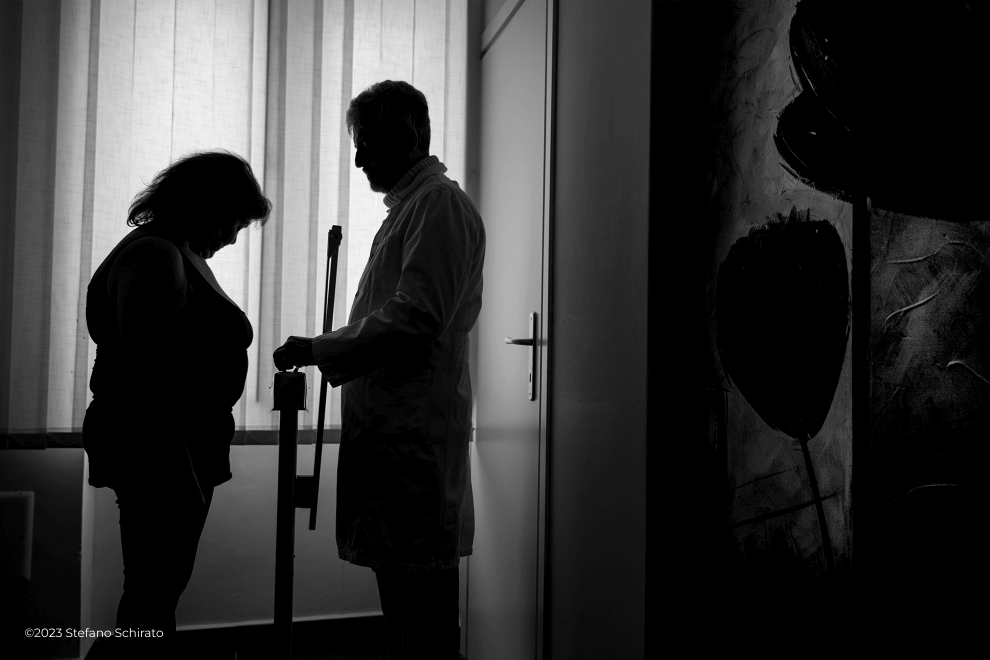
Eventually, symptoms usually bring people to their family doctor or other specialists. However, because some symptoms are not immediately recognized as Cushing’s-related, it may take a long time for someone to talk to a doctor specialized in the management of Cushing’s syndrome.4,7
Doctors will generally investigate Cushing’s syndrome by measuring cortisol levels in the body, and this can be done in a few ways.
The first method uses a mouth swab to measure levels of late-night salivary cortisol (LNSC) and is a common first step during the diagnosis. The second method measures for 24-hour urinary free cortisol (UFC) with a urine test, and the third method uses a blood test to measure cortisol levels after taking a low dose of a medication called dexamethasone. This is known as a dexamethasone-suppression test (DST).5
A diagnosis can usually be made from the results of these tests, but it is not always a simple journey for patients from when symptoms first appear to when they are tested for Cushing’s syndrome. In fact, due to the wide range of Cushing’s symptoms, patients can often wait 5-7 years from the onset of symptoms to diagnosis.6
Because Cushing’s syndrome can cause greater impact the longer it goes untreated, it is important to speak to a doctor as early as possible when symptoms appear. The earlier doctors can diagnose and start treatment, the lower the risk of potentially irreversible impacts from high cortisol levels.6,7
Experiencing signs or symptoms?
If you are experiencing signs or symptoms, speak with a doctor. You can find further resources on Orphanet.
Have you been diagnosed with CS?
Connect with the World Alliance of Pituitary Organizations (WAPO).
Further useful links:
Follow us on social media
The impact of Cushing’s Syndrome on one person can be very different to the next. Monitoring your disease journey and keeping your physician and family updated may be a helpful way to see changes over time.
Help your family and friends to better understand Cushing’s syndrome by sharing this website and encouraging them to keep up with the conversation on social media by following #ThisCushing on Twitter and LinkedIn.

